Lower Limb Therapies
Lower extremity peripheral artery disease (PAD) affects 12% to 20% of population over the age of 60 years and older. The most significant risk factors for PAD are hyperlipidemia, hypertension, diabetes mellitus, chronic kidney disease, and smoking; the presence of three or more factors confers a 10-fold increase in PAD risk. Intermittent claudication is the hallmark of atherosclerotic lower extremity PAD, but only about 10% of patients with PAD experience intermittent claudication.
A variety of leg symptoms that differ from classic claudication affects 50% of patients, and 40% have no leg symptoms at all. Current guidelines recommend resting ankle-brachial index (ABI) testing for patients with history or examination findings suggesting PAD. Patients with symptoms of PAD but a normal resting ABI can be further evaluated with exercise ABI testing. Routine ABI screening for those not at increased risk of PAD is not recommended.
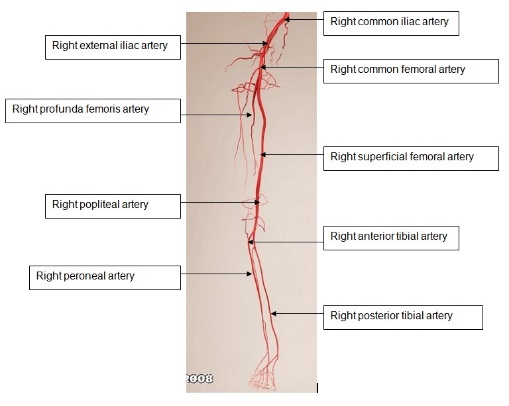
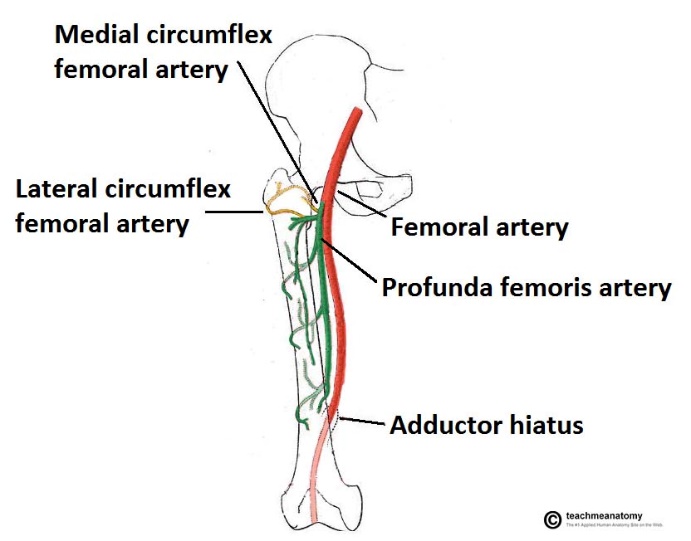
The main artery of the lower limb is the femoral artery. It is a continuation of the external iliac artery (terminal branch of the abdominal aorta). The external iliac becomes the femoral artery when it crosses under the inguinal ligament and enters the femoral triangle.
After exiting the femoral triangle, the femoral artery continues down the anterior surface of the thigh, via a tunnel known as the adductor canal. During its descent the artery supplies the anterior thigh muscles.
The adductor canal ends at an opening in the adductor magnus, called the adductor hiatus. The femoral artery moves through this opening, and enters the posterior compartment of the thigh, proximal to the knee. The femoral artery is now known as the popliteal artery.
The popliteal artery descends down the posterior thigh, giving rise to genicular branches that supply the knee joint. It moves through the popliteal fossa, exiting between the gastrocnemius and popliteus muscles.
